(In recognition of World Keratoconus Day, Dr.Deo Singh of the Ophthalmological Society of the West Indies shares a patient’s guide to Keratoconus)
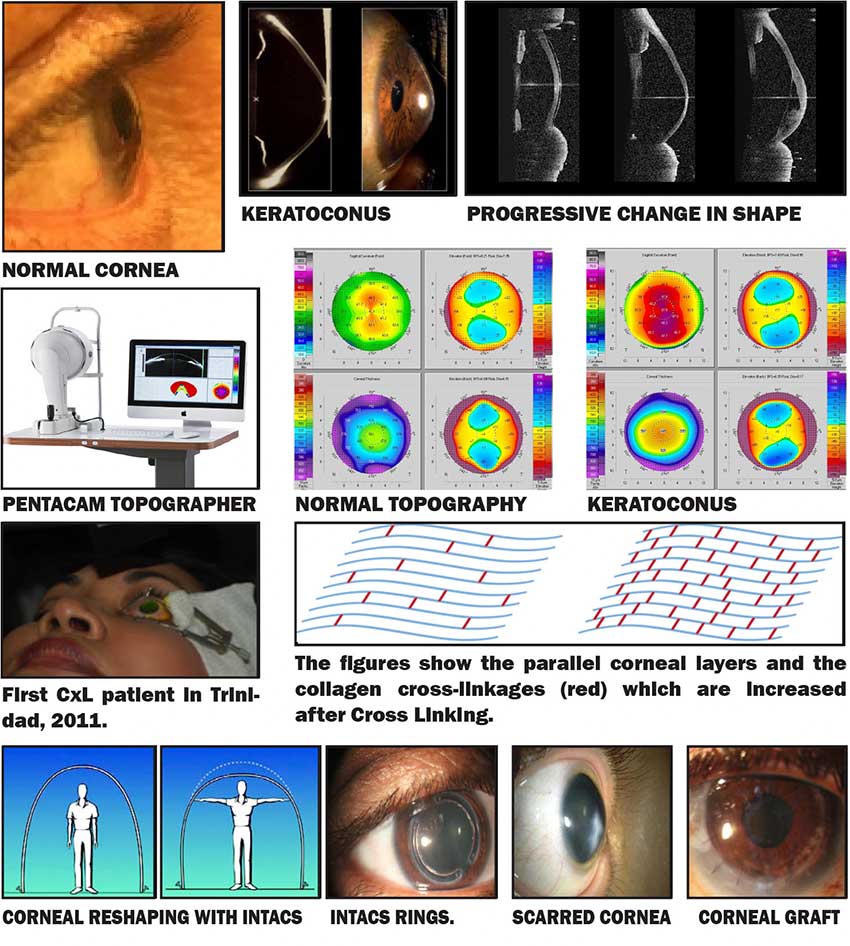
KERATOCONUS (or KC) is a non-inflammatory condition in which the normally round front surface of the eye, the cornea, becomes increasingly steeper (more highly curved).
It results in stretching, thinning and irregularity of the cornea, increasing myopia (short-sightedness) and irregular astigmatism. Vision becomes increasingly blurred. Vision may initially be improved by spectacles but later contact lenses are required.
Severe cases appear like the tip of an ice cream cone, i.e. conical. It may progress to scarring of the cornea requiring a corneal graft (transplant) operation to improve vision. KC often starts in the teens and progresses until the late twenties to thirties when it stabilizes or shows a reduction in the rate of progression.
HOW COMMON IS KERATOCONUS:
Keratoconus accounts for 60% of corneal transplants in Trinidad and Tobago.
CAUSATIVE FACTORS:
• Allergic conditions like Asthma*, Hay Fever, Sinusitis (the commonest associated factor in T&T is asthma.)
• Itchy Eyes and Eye Rubbing
• Heredity
SYMPTOMS:
• Blurred vision
• Distorted vision
• Needing to hold reading material close to the eyes
• Sensitivity to glare
• Multiple images or ghosting
• Frequent changes of spectacles or contact lenses
DIAGNOSIS
The diagnosis is suspected from:
• History of frequent changes in spectacle or contact lens prescription
• Progressive blurring of vision
• Increasing astigmatism
• Itching and rubbing of the eyes
• Family history of keratoconus
Corneal Topography
• This is a non-invasive method of mapping the curvatures of the corneal surfaces, assessing the degree of deviation from the normal cornea. Modern Topographers, like the Pentacam used, gives detailed point-to point information of curvatures of the front and back surfaces and of the thickness of each point on the cornea.
• The cornea is normally responsible for two-thirds (2/3) of the focusing power of the eye. Its topography is, therefore, very important to its function and the quality of vision.
MANAGEMENT:
• Allergy treatment
• Specific management of the individual patient depends on the severity and age of the patient
• In early cases, spectacle or contact lens correction and monitoring by repeat Topography
PREVENTIVE TREATMENT:
Corneal Crosslinking Keratoconus – Introduced to Trinidad and Tobago at CEI 2008
Corneal Crosslinking is now considered the first line of treatment for Keratoconus.
Ultraviolet corneal crosslinking (CxL) is the only treatment shown to slow the progression of keratoconus. It must be considered as the first line of treatment, especially in young patients, at diagnosis and before complications of the disease or contact lenses occur. It reduces the need for corneal transplant surgery in keratoconus. CxL is a painless office procedure, under anaesthetic drops, not requiring injections, uses a special preparation of Riboflavin (Vitamin B2) drops and a low dose UV light. Treatment takes 45 minutes to an hour.
It results in strengthening of the cornea that becomes more resistant to progressive deformation.
Strict criteria are used to determine the suitability of a given cornea for treatment. If the cornea has become too thin or scarred, then crosslinking will be less useful and corneal transplant surgery will be needed. Every young keratoconic patient must be referred to the Ophthalmologist for screening and for cornea crosslinking before being fitted with spectacles or contact lenses. These lenses compensate for the focusing deficiency caused by the abnormality in corneal shape. Spectacles and contact lenses DO NOT correct or treat the keratoconus and keratoconus often progresses (gets worse) in spite of contact lenses.
Contact lenses are often intolerable, do not fit properly, fall off the eye and do not give good vision as keratoconus gets worse. In more severe cases of keratoconus, wearing contact lens may contribute to scarring of the cornea.
INTACS IMPLANTS are crescent shaped segments of similar material to intraocular lenses used in cataract surgery. They are implanted into the cornea in a procedure under local anaesthetic. They serve to reshape (flatten) the very steep cornea, thereby improving vision. They also add structural stability.
INTACS should not be used in keratoconus patients who can achieve functional vision on a daily basis using contact lenses, are younger than 21 years of age, do not have clear central corneas, and have a corneal thickness less than 450 μ at the proposed incision site.
Corneal transplants, also known as corneal grafts, or keratoplasties.
Full Thickness Corneal Transplant (also called Penetrating Keratoplasty – PK) is done when there is significant corneal scarring.
Partial Thickness Corneal Transplant surgery (Deep Anterior lamellar Keratoplasty – DALK) is done in earlier cases when it is not possible to get functionally comfortable vision with contact lens wear and there is only superficial scarring. DALK is an advanced form of partial thickness corneal transplants that is specially-suited for Keratoconic patients who do not have advanced scarring of the cornea because it protects against graft rejection and minimizes the need for a repeat graft in later years.
DALK advantages:
i) Fewer problems with rejection
ii) Greater wound strength
iii) Reduced re-graft rate for young patients













