Introduction
With funding now in place, Saint Lucians, especially those living in the south, will be hoping the nightmarish St. Jude Hospital Reconstruction Project (SJHRP) experience is nearing its end. Unquestionably, such an end is deeply desired. When it is achieved, I will be deeply relieved. However, I feel certain I will not be able to celebrate, as it’s unlikely my mind will ever be purged of the sadness, shame, and even anger this project has caused me.
Lowest Point
Perhaps the lowest point of my anguish came at a World Bank restaurant in Washington D.C. circa 2017. There was a vacant seat at my table, which I readily offered to a Latina, with a plate-full, tray in her upraised hands. We introduced ourselves. She worked with Mexico’s cooperation agency. After a few spoonsful of soup, she asked me about the status of the SJHRP. I must have shown surprise at her interest. She quickly explained that her country had gifted a morgue to the hospital and was eager to see it completed. I did not know this. Shame weighed heavily on me, as I apologized for the delay, which I sinfully attributed to various “Acts of God.” Mea Maxima Culpa! I shared with her my understanding that the hospital was about 80% complete and that equipment was already being procured. As I walked back to my office, I asked myself: how it is that a country, with two Nobel Laureates, a wealth of accomplished construction expertise, and an impressive portfolio of complex, infrastructure projects—including a water dam and reservoir, cruise ship piers and a 126-bed hospital—is unable to build another smaller hospital? Churchill’s answer to a question put to him about the future disposition of post-war, Russia came to mind: “It is like a riddle, wrapped in a mystery, inside of an enigma” he’d said.
Building a Learning Society
To err is human. Because Governments are run by people, errors will occur. However, every error produces lessons which must be fully absorbed, to ensure it is not repeated. For this reason, we must remove our subjective, partisan lenses and undertake an unfiltered, objective assessment of what transpired with the SJHRP. It’s my hope this 3-part commentary will contribute in some small way towards this goal. In this first part, I revisit the arguments for and against a 2-hospital model. In part 2, I examine the bigger picture, including how we might fulfill a long-term vision for secondary health care. In part 3, I examine some key lessons from the approach to the SJHRP.
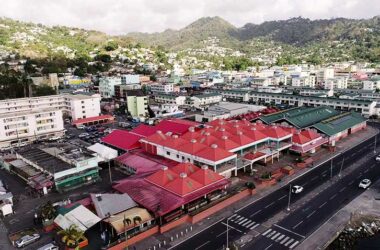
A brief history of the SJH
The SJH has a rich history dating back to the 1940s when it served as a US military hospital. Upon the departure of the Americans, it was shuttered until the mid-1960s, when it was reopened as a community hospital, run by the Sisters of the Sorrowful Mother. In 2003, the Government assumed responsibility for its management. At that time, SJH was a small, 88-bed, secondary care hospital that provided approximately 40,000 persons in the south of the island, with inpatient and outpatient, clinical and accident and emergency (A&E) services. Universally, secondary care hospitals provide specialized care for patients with severe or complex health conditions, such as cancer, pneumonia, sudden infections, and broken limbs.
The Health Reform Commission (HRC) Perspective.
For about six months in 2004, I was honored to have been a member of an HRC appointed by the Cabinet of Ministers, to review the terms and conditions of work of doctors and nurses in the public health service. The HRC was chaired by Sir Richard Haynes, (deceased), a renowned physician, and former Minister of Finance of Barbados, who had chaired a similar body in his country. Other members were, Mrs. Jennifer Astaphan, who was then Executive Director of the Caribbean Centre for Development Administration (CARICAD), and Dr. Barbara Johnson (deceased), who was a well-respected, pediatrician in Jamaica. As part of its work, the HRC took a detailed look at the governance of SJH, including its financial management, recruitment and retention of medical staff, and fee collection system.
After inspecting the facility, we immediately recognized it would “…require substantial upgrading to deliver quality, secondary care services, at the same level envisaged for the new hospital (later to be known as the ‘OKEU’ in Castries.” Also, we noted that a considerable amount of money was being spent on maintaining and repairing age-related defects at the facility. Despite these physical ailments, we considered SJH to be a well-run facility that seemed, “…relatively free from the negative cultural influences that afflicted Victoria Hospital (VH).” There were fewer complaints from the public and staff about its operations. Many users commented that it had a “friendlier” atmosphere and a more business-like approach to management, than VH. While in many instances, it charged higher fees than VH for the same services, more of its patients paid their bills, in cash and in-kind, resulting in higher revenue than at VH.
The Two Hospitals Model
Reference documents given to us included the final report of a Health Sector Reform Committee (HSR, 2000), led by Dr. Stephen King—which we considered an excellent report—and a Health Sector Study (2001). Both documents endorsed a “two hospitals” model for the island. The HSR report recommended that the hospitals “…function in an equivalent manner providing an equivalent service” with a caveat of sorts, that “lessons from one should be heeded in the design of what is appropriate, feasible and effective in the other.” We understood this to mean that the design of the OKEU, which was well-advanced, would influence the design of the SJH, in terms of scope of services, and financial and operational feasibility. Shockingly, the authors of the latter report, admitted their recommendation for 2 hospitals “…was not primarily based on planning, quality, or efficiency arguments.” We took a contrary view and approach. We believed—as hinted in the first Report, that the number of beds at the new hospital (OKEU) —among other factors, would heavily determine the future of SJH. At the time, no final decision had been made on this. There was talk of the OKEU having between 146 and 185 beds. We strongly urged that every effort should be made to achieve 185 beds. I will come back to this.
The main argument put to us for retaining SJH as a secondary care hospital, was distance (30 miles) and time (60-75 minutes), for southerners to get to the VH/OKEU. We did not see this as a compelling medical argument. The fact that patients from all over the island often sought specialist, medical attention at SJH undermined that argument. Further, we noted that for those living in the north, getting to VH (12 miles) can take between 45 minutes to an hour, depending on traffic.
In 2004, the average bed occupancy rate (BOR) at SJH was about 45%, meaning that less than half of its 88 beds were regularly occupied. While it may be argued that this excess capacity would cater for spikes in demand from a growing population in the south, the most critical factor in the functioning of any hospital is the availability of qualified, and experienced health personnel. As an example, the universally recommended, nurse-to-patient ratio in a hospital, ranges from 1:2 for an intensive care unit (ICU), to 1:4 for medical/surgery wards. Thus, we thought it would be unwise to duplicate the deployment of these limited resources at both hospitals. We were encouraged in this view by two factors: (1) SJH relied heavily on voluntary, specialist services from overseas; and (2) trends in healthcare pointed to secondary care being delivered, more on an out-patient basis (70%), than in-patient basis, (30%). We believed the demand for in-patient care would likely decline, if: (a) adequate facilities for geriatric care and expanded surgical facilities are provided; and (b) there is a robust and effective primary healthcare strategy and system. Here, we noted the positive impact of the Gros-Islet Polyclinic (GIP) in providing a higher order of primary health care, than the standard health (and wellness) centres. In our view, in many respects, the GIP functioned as an outpatient clinic to Victoria Hospital. We were puzzled that more polyclinics had not been built since then.
Regional Comparisons
The HRC reviewed the status quo in other Caribbean countries. It noted that since 1964, Barbados has had one, large, general hospital—the Queen Elizabeth Hospital (QEH) which doubles as a teaching hospital of University of the West Indies (UWI. In 2004, the QEH had a BOR of 120%. Presently, it has a bed capacity of 600 for a population of about 281,000. Its A&E department has 20 doctors serving approximately 45,000 patients annually. Over the past 3 decades, successive administrations committed to rebuilding the facility. Various physical alterations have been made but a total rebuild has not happened. It is noteworthy that under Barbados’ socialized healthcare model, its people receive free healthcare, at an average annual cost of about US$115 million. Jamaica too, provides free health care to its 2.8 million people. It has 5,000 public hospital beds across its 24 public hospitals—including the University Hospital of the West Indies—and 200 beds in 10 private hospitals. Its hospitals are classified as type A, B or C. Type A hospitals such as the Kingston Public Hospital and Cornwall’s Regional Hospitals provide comprehensive, secondary, and tertiary healthcare, and are the final referral points for public and private hospitals. In Type B facilities, there are restrictions on the scope of specialist services provided.
The HRC’s Recommendation
After considering key, relevant medical, planning, quality, cost, and efficiency factors, the HRC recommended that the ideal, medium, to long-term future for SJH is as a facility that: (1) shares specialist services with the OKEU; (2) provides diagnostic services of a modern, expanded, Polyclinic; (3) has an AED with adequate bed capacity to support stabilizing serious cases; (4) is supported by an adequate and efficient ambulance service. This would be akin to a Type-B facility in Jamaica, or a Level-3/4 facility based on international classification.
Current Stressors
Since 2004, the situation has changed somewhat. There’s been a manifold increase in population growth in the south, as well as in demand for emergency care, spawned by gang violence, and a spate of traffic accidents. In its current state, SJH is unable to adequately deal with this spike in cases, and patients are sometimes transferred to the OKEU. However, such transfers would likely still have occurred if SJH was fully functional, as there would be times when demand for its services would outstrip its coping capacity. Another important consideration is the SJH’s role relative to Hewanorra International Airport (HIA). Here, the ideal, strategic response would not be to build an over-sized, AED that is underutilized for long periods, but rather, to have a clear, well-tested, emergency response plan, that includes the OKEU and Soufriere hospitals and health centres in the southern half of the country. The number and the condition of available ambulances in the south, does not suggest all elements of an effective response plan are in place.
Conclusion
As things now stand, the die has been cast, and hopefully for better than for worse, Saint Lucia will soon have two secondary care hospitals, an hour’s drive apart, with a total capacity of about 220 beds. In next week’s commentary, I examine pertinent operational and financial viability issues and how they might be addressed.